Information for Providers
Many women who have been diagnosed with cancer think preserving their fertility is important and want information about their options. However, patients may not feel comfortable bringing up fertility issues.
Introduction
Understanding there are fertility preservation options available and referring at-risk patients in a timely manner to specialists can improve patients’ emotional outlook and future quality of life. However,
- Patients may not be aware of their options for preserving fertility.
- Patients may be focused on their cancer diagnosis and unable to think about fertility or the possibility of having a future family.
- Women may later regret not considering fertility issues prior to starting cancer treatment.
- Even women with a poor prognosis may want to consider fertility preservation.
Fertility Preservation - Where Does It Fit?
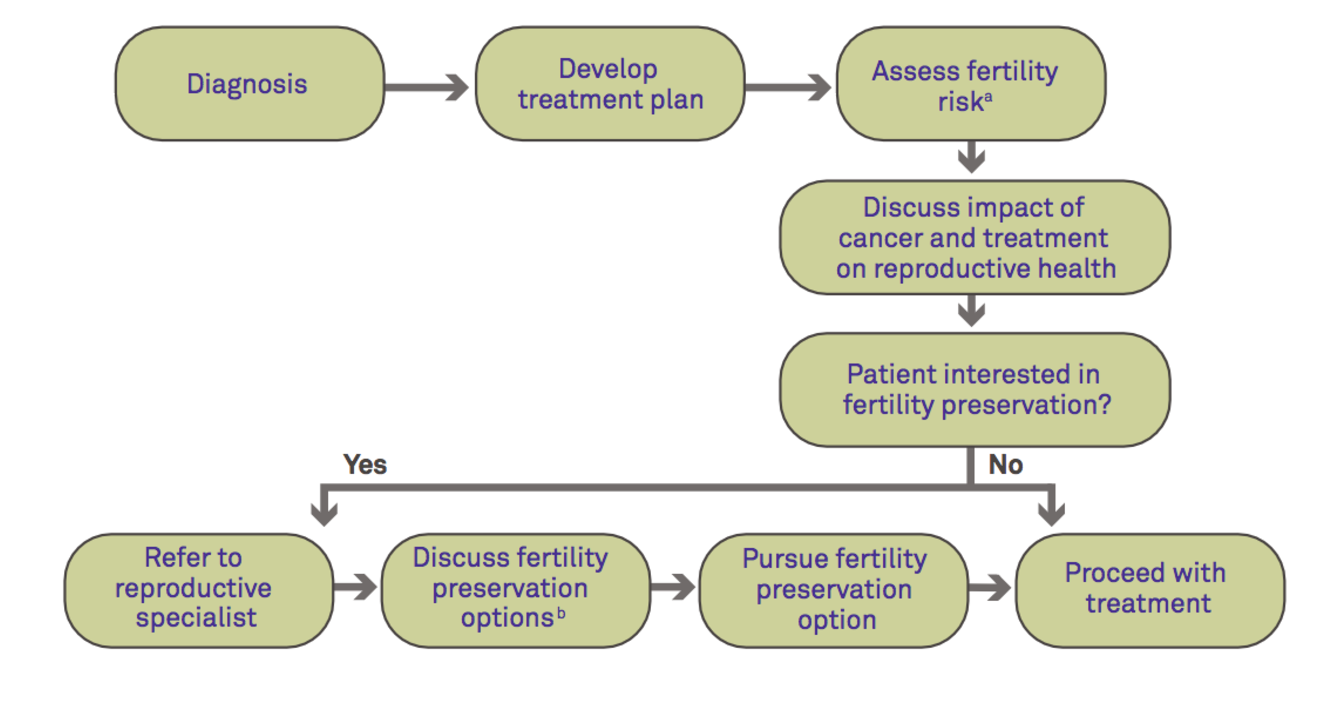
a) See table below
b) See figure below
Options for Fertility Preservation
- The following table gives a brief description of options available to women who wish to preserve their fertility.
- The American Society of Clinical Oncology and American Society for Reproductive Medicine recommend, when possible, at-risk patients be referred to a fertility preservation specialist prior to starting cancer treatment.
- Several resources are listed on the reverse that can help you and your patients locate a fertility preservation specialist.
- Remember there are other ways to build a family after cancer if we are unable to preserve your fertility now. Talking with a specialist can help you explore other options that might be right for you.
| Option | Definition | Timing | Time Requirement | Other Considerations |
|---|---|---|---|---|
|
Embryo Banking
|
Ovarian stimulation; Harvesting eggs, IVF and freezing of embryos | Before or after treamtment | 10-15 days outpatient surgical procedure | Need partner or sperm donor |
| Egg Banking | Ovarian stimulation; Harvesting and freezing of unfertilized eggs | Before or after treamtment | 10-15 days outpatient surgical procedure | |
| Ovarian Tissue Banking (Experimental) | Surgical removal of ovarian tissue and processing of tissue for freezing | Before or after treamtment | Outpatient surgical procedure | Autotransplantation of tissue has produced live births; studies ongoing for IVFM |
| Radiation Shielding | Use of shielding to reduce scatter radiation to the ovaries | During treatment | In conjunction with radiation treatments | Does not protect against effects of chemotherapy |
| Ovarian Transposition | Surgical reposition of ovaries out of radiation field | Before treatment | Outpatient procedure | |
| Radical Trachelectomy | Surgical removal of the cervix with preservation of the uterus | Before treatment | Inpatient surgical procedure | Limited to early stage cervical cancer |
| Ovarian Suppression (Experimental) | GnRH analogs used to suppress ovaries | During treatment | In conjunction with chemotherapy | Data are mixed on the effectiveness of this option. |
Starting the Conversation
Discussing fertility preservation is important. These key points can help start the conversation:
- Cancer and cancer treatment may affect your fertility.
- Based on your treatment plan, your risk of infertility is [high, moderate, low] (see table below).
- Although it may not be on your mind now, it is important to discuss fertility before you begin treatment.
- You may have options for fertility preservation before you begin cancer treatment (see table above).
- Not all women experience infertility after cancer treatment, however it is still important to explore your fertility preservation options before treatment.
- I can refer you to a fertility preservation specialist if you would like to discuss your options further.
Cancer Therapy and the Risk of Infertility
The following table classifies various cancer therapies and regimens based on their known infertility risk in women (defined as permanent amenorrhea).
While this table provides general guidelines, each patient is different and treatment may impair their fertility differently.
| High Risk |
|
|---|---|
|
Intermediate Risk |
|
| Low Risk |
|
| No Risk |
|
| Unknown Risk |
|
Table adapted from Fertile Hope, an initiative of LIVESTRONG; Cancer and Fertility: Fast Facts for Reproductive Professionals (2008); and Meirow D, et al. Clin Obstet Gynecol. 2010;53:727-739.
CMF=cyclophosphamide/methotrexate/fluorouracil • CEF=cyclophosphamide/epirubicin/fluorouracill • CAF=cyclophosphamide/adriamycin (doxorubicin)/ fluorouracill • MOPP=mechlorethamine/oncovin (vincristine)/procarbazine/prednisonel • MVPP=mechlorethamine/vinblastine/procarbazine/prednisolonel • COPP=cyclophosphamide/oncovin/procarbazine/prednisonel • ChlVPP=chlorambucil/vinblastine/procarbazine/prednisolonel • EVA=etoposide/vinblastine/\ adriamycinl • BEACOPP=bleomycin/etoposide/adriamycin/cyclophosphamide/oncovin/procarbazine/prednisonel • ABVD=adriamycin/bleomycin/vinblastine/ dacarbazinel • AC=adriamycin/cyclophosphamidel • CHOP= cyclophosphamide/hydroxydaunomycin/oncovin/prednisonel • COP= cyclophosphamide/oncovin/ prednisonel • MF=methotrexate/5-fluorouracil
Resources
For more information about infertility risk, fertility preservation options for women diagnosed with cancer, and how to locate and refer your patients to a fertility preservation specialist:
- Visit SaveMyFertility.org
- Call the FERTLINE: 866-708-FERT (3378)
- Visit the Oncofertility Consortium® Web site
- Use the online Clinic/Center Finder to find the fertility preservation center closest to you.
References
- The Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril. 2013; 100:1224-31.
- De Vos M, Smitz J, Woodruff TK. Fertility preservation in women with cancer. Lancet. 2014;384:1302-10.
- Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360:902-911.
- Loren AW, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013; 31: 2500-10.
- Meirow D, Biederman H, Anderson RA, Wallace WH. Toxicity of chemotherapy and radiation on female reproduction. Clin Obstet Gynecol. 2010;53:727-739.
- JM Letourneau, EE Ebbel, PP Katz, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012; 118:1710–1717.
- Levine JM, Kelvin JF, Quinn GP, Gracia CR. Infertility in reproductive-age female cancer survivors. Cancer. 2015;121(10):1532-9.
- Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Hum Reprod Update. 2009;15:587-597.
- Woodruff TK. The Oncofertility Consortium—addressing fertility in young people with cancer. Nat Rev Clin Oncol. 2010;7:466-475.

